Hello! Jada Shapiro here, passionate maternal health expert, longtime doula and founder of Boober, a platform where expectant parents and new families find classes and care providers to help them thrive from pregnancy to postpartum. I am dedicated to supporting expecting and new parents through every step of their journey from pregnancy to postpartum. With over two decades of experience as a birth and postpartum doula and a caring, evidence-based approach, I guide moms and parents with wisdom and understanding, ensuring they navigate each stage of growing their family with confidence and empowerment.
Postpartum pooping may not be a glamorous topic, but it holds immense importance in the realm of postpartum recovery. As a postpartum doula who is there with families in the earliest moments and days of their new role as a parent, I understand the significance of ensuring comfortable and regular bowel movements during this delicate phase. The postpartum period brings about profound physical and emotional changes, and addressing any pre-first-poop fears and any actual discomfort or irregularities in pooping is crucial for overall well-being. My expertise lies in providing caring support and practical guidance to help pregnant and new parents embrace this aspect of recovery, fostering more complete healing from the inside out, and setting the stage for strong bonds and a transition to postpartum where people thrive, not just survive!
Table of Contents
- How Long Does It Take To Poop Postpartum?
- How Does Giving Birth Affect Poop?
- How To Prepare For Your First Postpartum Poop
- Common Postpartum Poop Problems
- When To See a Doctor
- Final Words from a Doula
How Long Does It Take To Poop Postpartum?
Your first postpartum bowel movement typically occurs between 3-5 days after childbirth. But there are factors that cause this to vary, such as:
- Your usual bowel movement pattern. Are you a super frequent pooper? Or a every-few days kind of pooper?
- The details of your labor and delivery. Did you have a long labor with no eating for days? Or were you enjoying nibbles throughout?
- Whether you took any constipating medications. Like narcotics during labor or a potentially constipating supplement like iron.
- Whether you had a soft bowel movement or diarrhea in early labor. If so, your body is already cleaned out, so it may take more time to build up to your next poop!
Worry about discomfort or complications can delay that first poop. However, many people find that their first postpartum bowel movement is less challenging than anticipated, especially if they prepare ahead of time and eat the right smooth-move foods and fluids after birth.
How Does Giving Birth Affect Poop?

Factors such as pain medications, hormonal changes, and alterations in diet or fluid intake during labor and postpartum recovery can also impact bowel function. While these issues typically resolve as the body heals and adjusts in the early postpartum period, practicing healthy poop habits and knowing what’s normal can help!
During labor, especially in the pushing stage, the pressure exerted on the rectum and surrounding muscles can lead to involuntary bowel movements. This is often referred to as "pooping while pushing." It's a natural occurrence due to the position of the baby's head pressing on the rectum as it descends through the birth canal.
Additionally, the process of childbirth, particularly vaginal delivery, can lead to stretching and while normal for most people, there can be potential damage to the pelvic floor muscles in some people. These muscles play a crucial role in bowel control. Weakening of these muscles post-birth can result in difficulties with bowel movements, including constipation or incontinence or challenges holding back gas at first.
Overall, while giving birth can temporarily affect bowel movements, these issues typically resolve as the body heals and adjusts in the postpartum period. However, it's essential for new mothers or birthing parents to practice self-care and seek support from healthcare providers if they experience persistent or severe bowel problems after childbirth.
Perineal Tears and Episiotomies
Before the fear of postpartum pooping sets in, most pregnant moms or new parents are worried about tearing or needing an episiotomy. While perineal tears or cuts affect up to 80% of women during childbirth, many of these tears may be so minor, they are barely noticeable. Whereas for others they are significant.
The difference between a perineal tear and an episiotomy is that one happens naturally (the tear), while the other is a medical intervention, in which your OB or midwife makes a surgical incision in the perineum (the space between your vagina and anus) to enlarge the vaginal opening. Episiotomy, no longer recommended as a routine, should only be used in serious situations such as:
- When the baby's oxygen supply is significantly compromised
- In certain cases where the baby is too large
- In complicated deliveries including breech births or shoulder dystocia, certain forceps or vacuum deliveries
Episiotomy can result in worse tearing, which is why it should be avoided unless absolutely necessary.
How to avoid an episiotomy:
- Hire a midwife or OB who rarely does them
- Take a childbirth class while pregnant to learn more about how to advocate for yourself so interventions like this aren’t overused
- Consider holding off on an epidural which can increase the need for forceps or vacuum which thus increases the likelihood of an episiotomy
- Also, ask your midwife or OB if they have any techniques known to decrease the likelihood of a tear, including warm compresses, counterpressure and position changes to facilitate rotation and ease of the baby like all fours or sidelying.
As a result of a tear or episiotomy, someone who just gave birth may experience pain, swelling, and discomfort in the perineal area postpartum, which can make the idea of bowel movements challenging and painful. The fear of aggravating the wound site may also lead to hesitation or avoidance of bowel movements, contributing to constipation or difficulty passing stools.
Loosened Pelvic, Rectal & Abdominal Muscles
Throughout pregnancy and labor and delivery, your pelvic, rectal and abdominal muscles have all loosened and adjusted to accommodate your growing baby. For vaginal births and cesarean sections, this holds true!
A pregnancy hormone called relaxin gets to work almost immediately — peaking during the first and last trimester of pregnancy — to increase elasticity of your tissues, ligaments and muscles. This is why your joints may ache and your back might hurt or why you sometimes easily pull a muscle from a quick step onto a dance floor! Relaxin stays in your body for many months post delivery, which is why you may still be feeling achy, wobbly or “loose.”
Your body has gone through something incredibly valiant and will need some time to put things back together and tone up its muscles again. The aches and pains in your vagina, pelvis, rectum and abs can affect your bowel movements, so try not to strain when on the toilet, and just like pushing your baby out, push your first poop out when it feels ready!! Let the sensation build, go when it’s time and don’t ignore the cue.
Pooping and Enemas During Delivery
Enemas during delivery are exceedingly rare nowadays but might be offered to stimulate labor or for those who prefer to minimize the chance of pooping while pushing. Rest assured, birthing staff are incredibly skilled at discreetly and quickly wiping away any poop that may occur, ensuring minimal disruption. In fact, a little poop during pushing is often a positive sign that you're effectively pushing.
Additionally, the body typically undergoes its own clearing process in the days leading up to birth, often through soft bowel movements or mild diarrhea. If you've had an enema or experienced multiple soft bowel movements during labor, it might reduce the urge to go after giving birth since your bowels are likely empty, especially if you hadn't consumed much during labor. Stay patient, stay hydrated, nourish yourself with warm broths and high-fiber foods, and trust your body to prompt its next bowel movement naturally.
Hormonal Changes and Stress
With a new human in the house depending on you for survival, your body recovering from delivery, and hormones fluctuating wildly, these combined challenges can exacerbate anxiety about pooping and experiencing postpartum constipation.
Post-birth hormonal changes and stress can affect your first postpartum bowel movement. Hormonal fluctuations, including the sudden drop in progesterone and estrogen levels, can lead to experiencing the "baby blues," characterized by mood swings, from joy to weepiness, and heightened emotions for up to 7-14 days. Prolonged symptoms or abnormal feelings may indicate a PMAD (postpartum mood and anxiety disorder) like postpartum depression or anxiety, both of which are treatable with professional help. Consulting with a midwife, doctor, or therapist who specializes in postpartum care is advisable in such cases. The drop in progesterone can also contribute to sluggish bowel movements and constipation. Stress hormones like cortisol can disrupt normal bowel function, making it more challenging to have a comfortable and regular first poop after giving birth. Managing stress through self-care practices and hiring helpful and caring support like a postpartum doula is known to reduce stress and PMADS.
How To Prepare For Your First Postpartum Poop
During Your Pregnancy
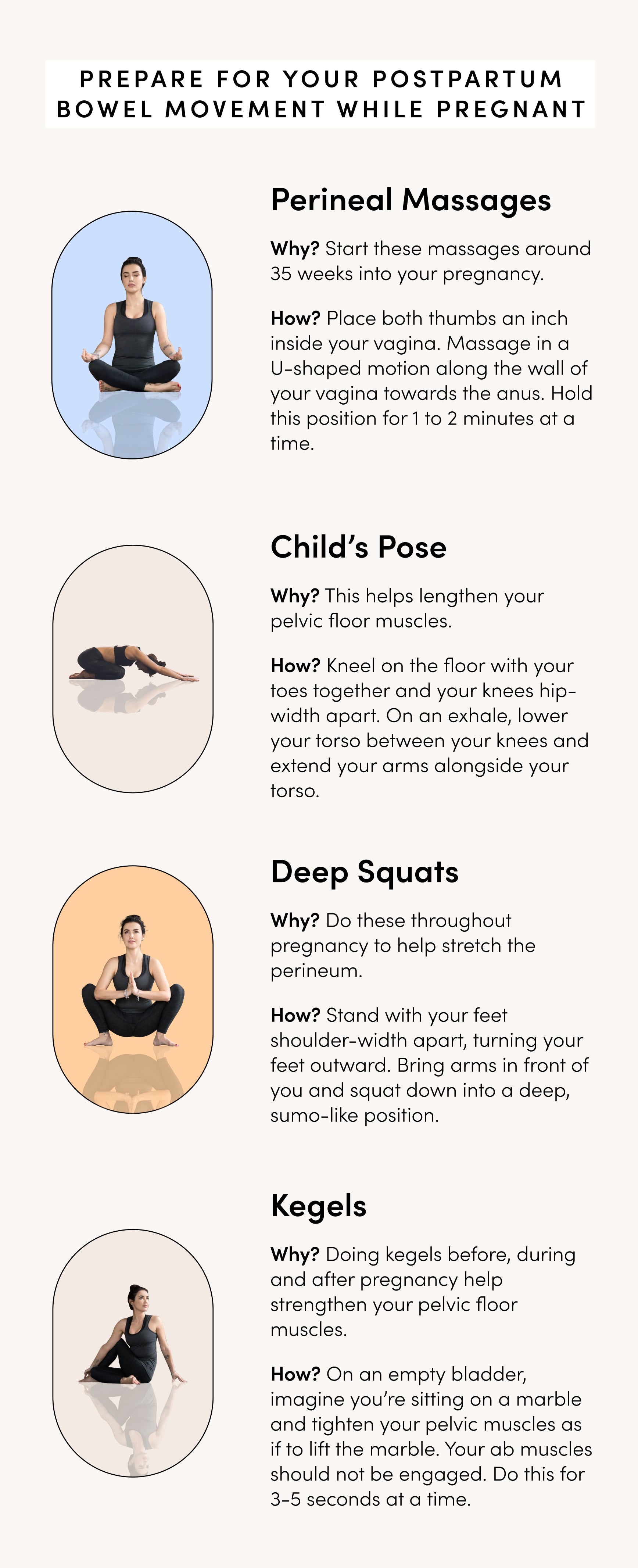
- Practice Perineal Massages. Prenatal Perineal massage helps you learn to tolerate the intense sensation you may feel when the baby's head emerges and also may ease your first postpartum bowel movement. You can talk to your midwife or doctor about whether they recommend this massage and you can start performing perineal massages anytime after 35 weeks of pregnancy.
- If your partner is performing the massage, they should face you, place both thumbs into the vagina, and then gently press down while slowly moving the thumbs apart, maintaining gentle downward pressure.
- If you are performing the massage yourself, lay down, relax your pelvic floor, and insert your clean, lubricated fingers to gently press down and move to each side. The stretch should feel gentle and may cause a slight burning sensation, but it shouldn't be extremely painful.
- Get In Child’s Pose. Child's pose helps maintain flexibility in key areas like the hips, back, and shoulders, which undergo significant changes during pregnancy. Additionally, it can alleviate lower back pain, release tension in the abdomen, and encourage deep breathing, promoting relaxation and enhancing overall well-being.
- Do Deep Squats. Getting into the deep squat position helps stretch the hips, relax and lengthen your pelvic floor muscles, and stretches the perineum—a three-in-one benefit! Keeping them toned and stretched during pregnancy can lower the risk of tearing, reduce the likelihood of postpartum incontinence, and potentially minimize trauma to the vagina.
- Kegels, Kegels, Kegels. Studies continue to show that doing kegels before, during, and after pregnancy can decrease the odds of postpartum incontinence and pelvic floor issues. People who have made a habit of doing pelvic floor exercises may have a slightly shorter active phase of labor! However, it's crucial to do kegels correctly and learn how to release and relax the pelvic floor, not just tighten or contract it. Take a prenatal pilates class or book a visit with a pelvic floor therapist trained to teach you how to do this correctly!
After Giving Birth

- Drink Lots of Water. As you embark on your postpartum pooping journey, it's essential to replenish your post-childbirth body with plenty of water and hydrating fluids like coconut water, nourishing teas, and warm broths. Water helps soften stools, making them easier to pass and reducing the likelihood of constipation.
- Eat Healthy Meals and Snacks. While it may be tempting to opt for quick, fast meals as a new mom or birthing parent, prioritizing nutritious options is key. Your first poops thrive on easy to digest, fiber-filled foods, so focus on snacks that support a sluggish digestive system, such as warm broths, whole grains, nuts, fresh fruits, and steamed vegetables.. Postpartum doulas love to prepare and serve you the most nourishing postpartum meals and snacks.
- Pamper Your Perineum. Immediately after delivery, nurses often use large ice packs in mesh postpartum undies to reduce swelling and alleviate pain. Once home, your postpartum doula, friend or family member, can assist you in preparing an herbal sitz bath or herbal steam.
“Padsicles” involve coating maxi pads with witch hazel, a known astringent, swelling reducer and hemorrhoid reducer (and optionally adding a few drops of lavender essential oil) before freezing them for later use. Just sit on a frozen padsicle after birth to provide relief.
- Use Stool Softeners. If you're able to consume high-fiber foods, plenty of broths, and ample water and nutritious beverages, you may not need them. However, if you tend to experience constipation it's advisable to consult your midwife or doctor about taking these pills. Stool softeners aren't laxatives, so you won't experience immediate urgency to use the restroom. Instead, they work to prevent stool from hardening, making it easier to pass when the time comes.
- Don’t Ignore the Urge to Go. If there's an urge to go, just like with pushing out a baby, take a deep breath, sit, and follow the urges you get. Holding in your stool for fear of passing it only prolongs or increases postpartum constipation you may be experiencing. Using a toilet stool and sitting with your feet raised will help your colon relax and make it easier for your stool to pass.
- Take Light Walks. Once you’re feeling up for it, taking light walks can make all the difference in your mood and gut groove. Plus, that bit of fresh air and light exercise even if it’s just for 10 minutes will activate your body and bowels, working wonders for your postpartum poop, and kicking that constipation to the curb!
Common Postpartum Poop Problems
Whether you're dealing with the discomfort of hemorrhoids or struggling with constipation and diarrhea, implementing effective strategies can help manage these concerns and improve digestive health during the postpartum period.
Postpartum Hemorrhoids
Hemorrhoids are a common occurrence postpartum due to the increased pressure on the rectum and pelvic area during childbirth, as well as hormonal changes that can relax the veins in the rectal area. To alleviate discomfort from hemorrhoids, it's essential to:
- Maintain good hygiene practices, such as gently cleaning the area with warm water after bowel movements
- Apply cold packs or witch hazel pads to the affected area to help reduce swelling and pain
- Incorporate high-fiber foods into your diet
- Stay hydrated
- Avoid straining during bowel movements
Some midwives swear by inserting a garlic clove into the anus for fast relief! Ask your midwife or doctor which treatment they recommend. If discomfort persists or your hemorrhoids get worse, tell your healthcare provider for further guidance and treatment options.
Postpartum Constipation
Constipation is a common postpartum issue due to various factors, including hormonal changes, dehydration, and reduced physical activity during recovery. The pressure of the growing uterus during pregnancy can also affect bowel function, leading to constipation after childbirth. To alleviate constipation, it's crucial to:
- Consume a diet rich in fiber from fruits, vegetables, whole grains, and legumes
- Stay hydrated by drinking plenty of water and other fluids
- Perform gentle exercises like walking or postpartum yoga to stimulate bowel movements
- Avoid delaying the urge to have a bowel movement
- Incorporate stool softeners or fiber supplements under the guidance of your healthcare provider
If you took any narcotic medication during labor or birth, you may be more likely to experience constipation. If constipation persists or becomes severe, consult with your healthcare provider for further evaluation and management.
Postpartum Diarrhea
Diarrhea can occur postpartum due to factors such as hormonal fluctuations, stress, dietary changes, and medications or antibiotics taken during labor or postpartum recovery. Additionally, the body may be adjusting to hormonal shifts and changes in gut bacteria after childbirth, leading to temporary digestive disturbances. To manage postpartum diarrhea, it's essential to:
- Stay hydrated by drinking plenty of fluids like water, herbal teas, and electrolyte-rich beverages
- Consume bland, easily digestible foods like bananas, rice, applesauce, and toast (the BRAT diet)
- Avoid spicy, greasy, or high-fiber foods that may exacerbate diarrhea
- Practice good hand hygiene
If diarrhea persists for more than a few days or is accompanied by other concerning symptoms, consult with your healthcare provider for further evaluation and treatment.
Postpartum Encopresis
Encopresis, or fecal incontinence, can occur postpartum due to various factors such as perineal trauma during childbirth like damage to the pelvic floor muscles or nerves (or both) during delivery, or from a tear or another injury to the anal sphincter, weakened pelvic floor muscles, or nerve damage.
Hormonal changes and medication use during labor or postpartum recovery can contribute to bowel control issues. To address encopresis, it's crucial to:
- Strengthen pelvic floor muscles and seek guidance from a pelvic floor therapist if needed
- Maintain a high-fiber diet
- Stay hydrated
- Establish a regular bowel routine
- Practice mindfulness techniques to reduce stress and anxiety
If encopresis persists or worsens, consult with your healthcare provider for further evaluation, medication, and treatment options.
When To See a Doctor
If you're experiencing persistent difficulty with bowel movements postpartum or are encountering symptoms such as severe pain, rectal bleeding, or abdominal distension, it's essential to seek medical attention promptly. These symptoms may indicate underlying issues such as bowel obstruction, hemorrhoids, or perineal tears that require medical evaluation and treatment.
If you have a history of gastrointestinal conditions like irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), or if you're experiencing symptoms like nausea, vomiting, fever, or unintended weight loss along with bowel problems, it's crucial to consult with your healthcare provider for comprehensive evaluation and management. Remember that timely medical intervention can help address underlying issues, alleviate discomfort, and promote better postpartum recovery.
Final Words from a Doula
Bringing a baby into the world is a monumental achievement, and the first postpartum bowel movement is just a small hurdle compared to what you've already accomplished! While discomfort and anxiety are common, they are typically temporary. Choosing a supportive midwife or OB who prioritizes perineal protection, practicing pelvic floor exercises and perineal massages during pregnancy, and hiring a birth doula to help navigate labor can all contribute to a smoother postpartum experience. Additionally, enlisting the support of a postpartum doula and having self-care products like calendula and Epsom salts on hand for sitz baths and padsicles can further ease discomfort and anxiety surrounding that first bowel movement after childbirth.
Postpartum preparation classes, and TUSHY products like the toilet stool and warm water bidet are lifesavers for postpartum parents with so many bidet enefits — they encourage healthy bowel movements and relief for your ever-deserving tender postpartum parts.
Frequently Asked Questions
Should you wipe after pooping postpartum?
The thought of touching such tender parts is scary. Using a warm water bidet spray is gentle and amazing (and super helps when you pee too because it dilutes your urine so any cuts or tears won’t sting as much) or use a travel bidet for a cheap, convenient way to clean your poop and reduce your pain!
Does breastfeeding affect a mother’s bowel movements?
For some people, yes! The amazing hormone oxytocin, which is released during lactation to move your milk (and which also creates contractions during labor, plus feelings of bonding and well-being!), can also stimulate contractions in the intestines. Additionally, nursing parents may experience changes in their diet and fluid intake, which can influence bowel movements.
How can I ease my postpartum poop?
To ease postpartum pooping discomfort:
- Focus on staying hydrated and incorporating fiber-rich foods.
- Practice pelvic floor exercises, such as Kegels, to strengthen and lengthen muscles and promote healthy bowel movements.
- Keep the perineal area clean using a bidet or portable bidet for gentle cleansing after bowel movements.
- Use a toilet stool to elevate your feet while sitting on the toilet for better alignment.
- Practice relaxation techniques to ease tension and reduce anxiety during bowel movements.
Remember to be patient with your body's recovery process, and consult with your healthcare provider if you experience persistent discomfort or other concerning symptoms.


















![Why It Feels Good to Poop [Poophoria Explained]](http://hellotushy.com/cdn/shop/articles/Poophoria_Explained.jpg?v=1611854103)








